I have a very clear memory of the events of July 29, 2004. We arrived at the medical university OB/GYN clinic and were taken into an ultrasound room. The technician was very nice and seemed genuine in her concern for Sherry’s comfort. Things seemed to be going well. The technician gave us an unofficial comment that told us the cyst was not a serious concern. The moments to follow began to change the mood of the room. The technician stated that she needed to verify something and left the room. She returned with another technician to verify what she saw on the ultrasound monitor. A few minutes later one technician left to get a doctor. This doctor brought in another doctor and a genetic counselor. Sherry and I noticed the tears starting to build in the original technician’s eyes. The doctor then broke the news. The technician had detected a fairly significant hole between the ventricles of our baby’s heart. This heart defect is referred to as a VSD (Ventricular Septal Defect).
I have a very clear memory of the events of July 29, 2004. We arrived at the medical university OB/GYN clinic and were taken into an ultrasound room. The technician was very nice and seemed genuine in her concern for Sherry’s comfort. Things seemed to be going well. The technician gave us an unofficial comment that told us the cyst was not a serious concern. The moments to follow began to change the mood of the room. The technician stated that she needed to verify something and left the room. She returned with another technician to verify what she saw on the ultrasound monitor. A few minutes later one technician left to get a doctor. This doctor brought in another doctor and a genetic counselor. Sherry and I noticed the tears starting to build in the original technician’s eyes. The doctor then broke the news. The technician had detected a fairly significant hole between the ventricles of our baby’s heart. This heart defect is referred to as a VSD (Ventricular Septal Defect).
This was all quite overwhelming to Sherry and me. At the time we had no idea that the VSD would be the least of our concerns. She was crying, the technician was crying, and I didn’t know what to do as tears flooded my face. The doctor said he was referring us to the Pediatric Cardiology Department in the main hospital for an echocardiogram to verify the findings. We waited while calls were made to get us in to Cardiology immediately.
This was the beginning of the end of the name game. Sherry and I decided that there were going to be enough surprises in the remainder of this pregnancy so we asked the technician to tell us the gender of our child. “It’s a boy!” We were excited! Now my list of names to choose from was cut in half. Even better, we could now refer to the baby as “he” instead of “the baby”.
The Pediatric Cardiology Department was able to see us that same day as requested by Sherry’s be OB/GYN. We made our way to Peds Cardiology in the rain. This was my first time stepping foot in the Medical University of South Carolina hospital. Entering the hospital was intimidating enough without the stress of the underlying purpose of our visit. The place was huge. It was bigger than any civilian hospital I had ever been in. Unlike us, most people were moving about as if they knew exactly where they were going. We finally found our way to the Pediatric Cardiology Department on the sixth floor of the Children’s Hospital in the maze of interconnected buildings.
We were met by a very friendly and compassionate staff. I didn’t know it then, but this was a scene that they had experienced before. We went into a room with a machine very much like the room we had been in at the OB/GYN clinic where the last ultrasound was done just hours before. The technician came in and spent what seemed like an hour taking pictures of our baby’s heart. The process was almost identical to an ultrasound from our perspective with the exception of the monitor showing only our son’s heart. Very few words were spoken. The technician finally got up and told us that the doctor would review the images and then come talk to us shortly. The doctor came in sooner than we expected. He was a very nice man who seemed as compassionate and sincere as everyone else we had talked to that day. He explained to us the details of our son’s heart defects. Yes, there appeared to be several of them. The most serious defect was referred to as an Interrupted Aortic Arch (IAA). The doctor said that the aorta, which carries oxygenated blood away from the heart, did not appear to be connected properly. Part of the aorta was believed to be narrowed or may even be missing. They were unable to tell the exact diagnosis with the angle of the two-dimensional picture from the echocardiogram. The doctor also reported that the PDA (Patent Ductus Arteriosus) was enlarged. The PDA is a natural bypass that allows the blood between the oxygenated and the less-oxygenated sides of the heart to mix while a baby is in the womb. Babies get their oxygenated blood from the mother until after birth, and the PDA helps mom’s blood mix with the baby’s blood.
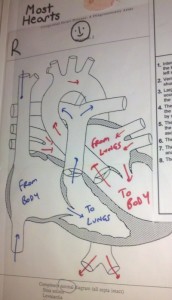
The doctor proceeded to tell us that if our son’s PDA closed after birth it could be fatal due to the suspected narrowing or restriction of the aorta. He told us that our son would require open-heart surgery shortly after birth. We asked for a better definition of “shortly”. He told us that our son would most likely require surgery within a week after he was born. These drawings were given to us to illustrate what they had found during the fetal echocardiogram. We would later learn how eerily accurate these drawings were even though there representing a child’s heart that was only about 22 weeks in womb.
The doctor went on to tell us that these heart defects would require medication called prostaglandins to be administered immediately after birth to help prevent the PDA from closing before the surgery could be performed. He told us that this drug could only be delivered through a central line. A central line is an IV-type line that runs through the baby’s belly- button or a central artery, and is threaded in as near as possible to the heart. This would allow the drug to be delivered to an area of the circulation system that would allow for the fastest distribution of the drug. He told us that these lines are normally inserted immediately after birth before the blood starts to clot in the veins that are fed by the umbilical cord.
The doctor took as much time as we needed to understand what he was explaining to us. He had drawings of a normal heart. He had another drawing of what he derived from the echocardiogram to illustrate what he believed our son’s heart looked like. He did give us a tiny bit of hope by telling us that we needed to follow the progress of these defects with more echocardiograms. There was a chance that things could get worse, but there was a chance that things could get better. By no means did the doctor give us a gleaming ray of hope that the defects would completely disappear.
Sherry and I were pretty overwhelmed at this point. The whole thing had really not sunk in for me just yet. The staff realized that we were near a state of shock. They told us to sit in the examination room as long as we needed before leaving. They offered their contact information for us to use to call with any questions that we had after we got home. They scheduled follow-up appointments for Sherry to have the echocardiograms throughout the remainder of the pregnancy to see if the defect had progressed in either direction. We finished our talk with the doctor and prepared to leave.
A nice lady from their office escorted us to the elevator. What happened next still gives me chills to this day. I started to have trouble breathing. My knees felt as if they were about to come out from under me. I grabbed the wall and asked if there was somewhere I could sit down. The lady walking with us immediately helped me into the nearest room. I sat down and began to sob uncontrollably. Sherry comforted me as she cried. I cried and gasped for air for a while. It seemed that nothing could stop it. The reality of the day’s events had finally caught up with me. I had no idea how to deal with what was happening to my young family. How could this happen? Our first child had nearly perfect health compared to this. Why was this happening to us? What had we done to deserve this? I had more emotions and questions in that moment than I can remember ever having in my life. I finally was able to gather myself enough to depart the sixth floor of the Medical University of South Carolina Children’s Hospital.
Caden is now seven years old and has endured many major surgeries including multiple heart surgeries, back surgeries, stomach surgeries, neck surgery and much more. He is still exclusively tube fed and has been given no hope of ever being able to nourish himself by mouth. He is expected to live a long life with proper medical treatment including regular cardiology check ups.
You can read Caden’s Page for the ongoing story of his life.